I recognize your anguish. Long COVID is new, and I will do my best to support you through this new and confusing illness. This is all I wanted to hear in my countless doctor’s visits. Some came close. The rest were baffled, given how healthy I was prior to a “mild COVID” infection.
I felt patronized by my own colleagues for trying experimental therapy. When activities of daily living are a strain, then engaging with people feels like too much. I am a critical care physician and feel lucky to have served on the pandemic frontlines in both India and the United States. I was vaccinated four times. Twice with Astra Zeneca Covishield while working with Doctors without Borders in Mumbai and twice with Pfizer in New York City.
I finally contracted COVID in January 2022 during the Omicron surge. My symptom was a persistent cough while working a night ICU shift. I had low-grade fevers, overwhelming fatigue, and malaise, and I even ordered my morning coffee. Living alone on the Upper West Side was so convenient. With largely normal vital signs, I felt confident of recovery. My urgent care telehealth doctor reassured me I didn’t need Paxlovid with such low-risk factors.
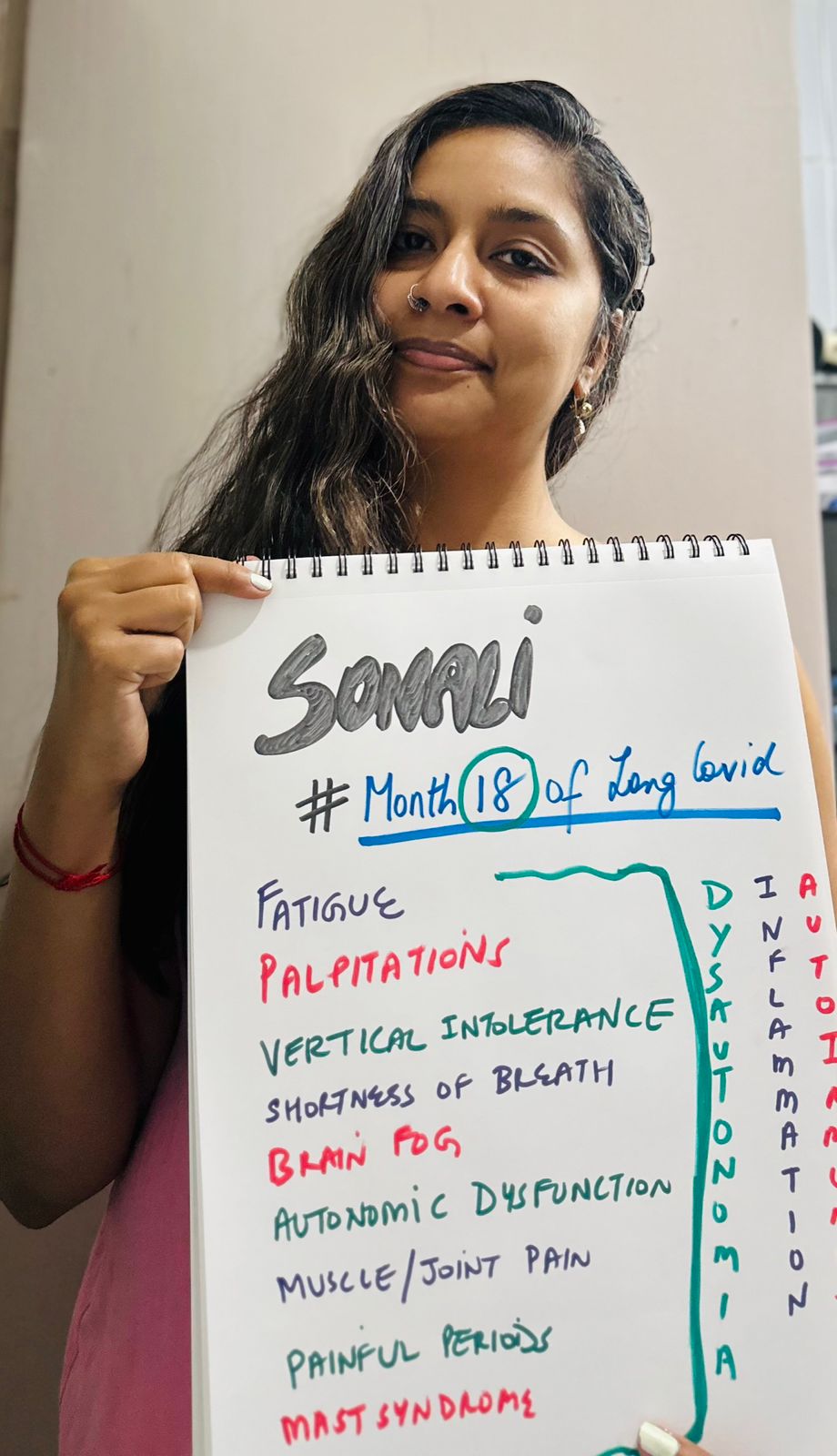
Two weeks later, I still felt profoundly fatigued and breathless and had palpitations and brain fog. I would slide in and out of my bathtub to bathe and had to sit down to dress myself. Walking around my 1,100-square-foot foot was a struggle. I went back to work, assuming post-viral fatigue would gradually improve. But I couldn’t stand for long during procedures and couldn’t take the stairs. I would lie down in the call room in between patients. Socializing halted, and I became increasingly isolated due to low energy reserves. Thus began the long COVID saga.
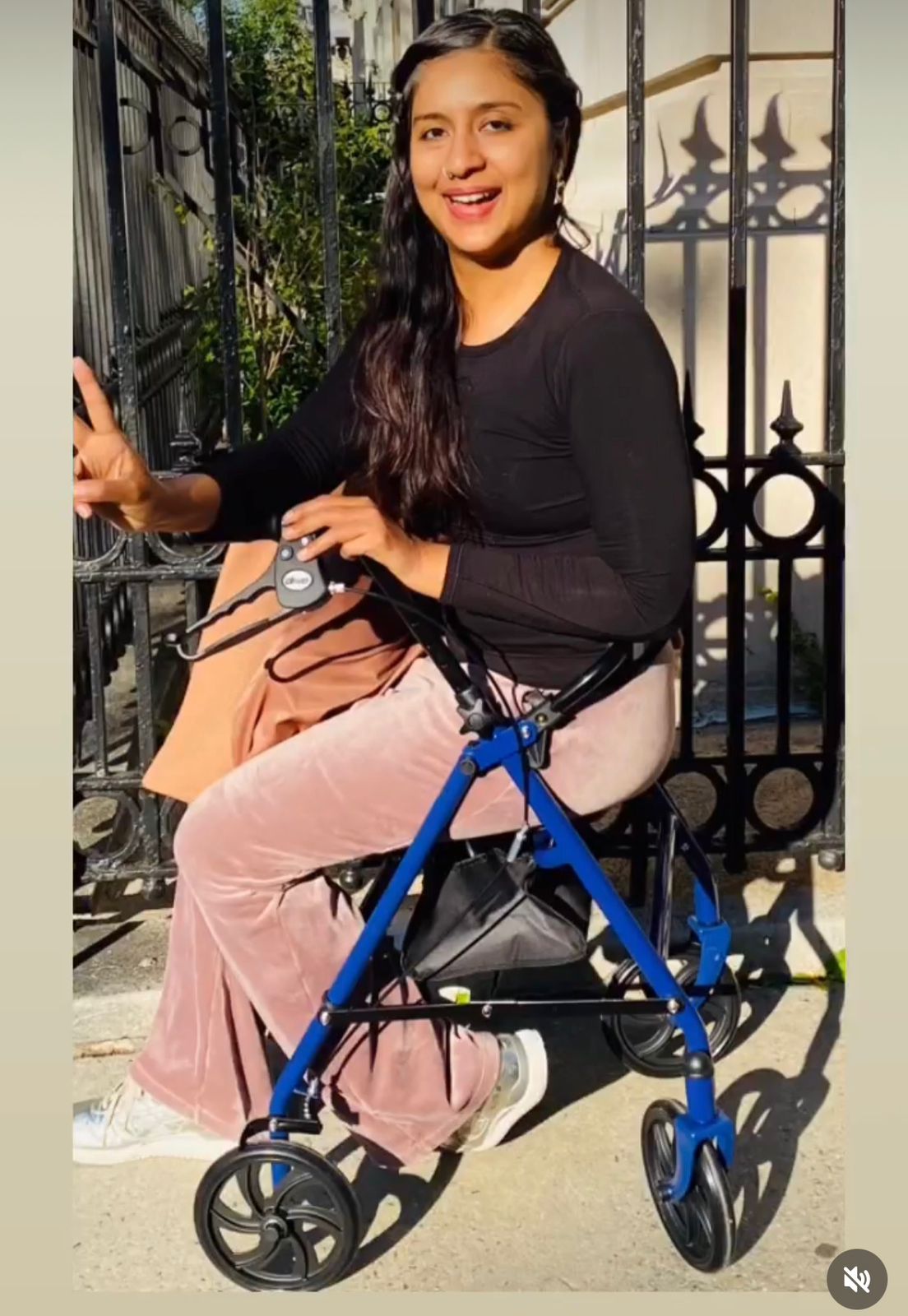
I normally walk fast like New Yorkers do and speak fast like Indians do. My life was active working at an academic hospital, and I only saw my doctor annually. I am a self-professed wellness junkie and strive to maintain meaningful relationships. Fast forward eighteen months, slow living is the norm. I compare myself to a low cellphone battery with limited functionality. Activities of daily living and gentle rehab take all day. I need help with meal prep, filling up my pillbox, and errands.
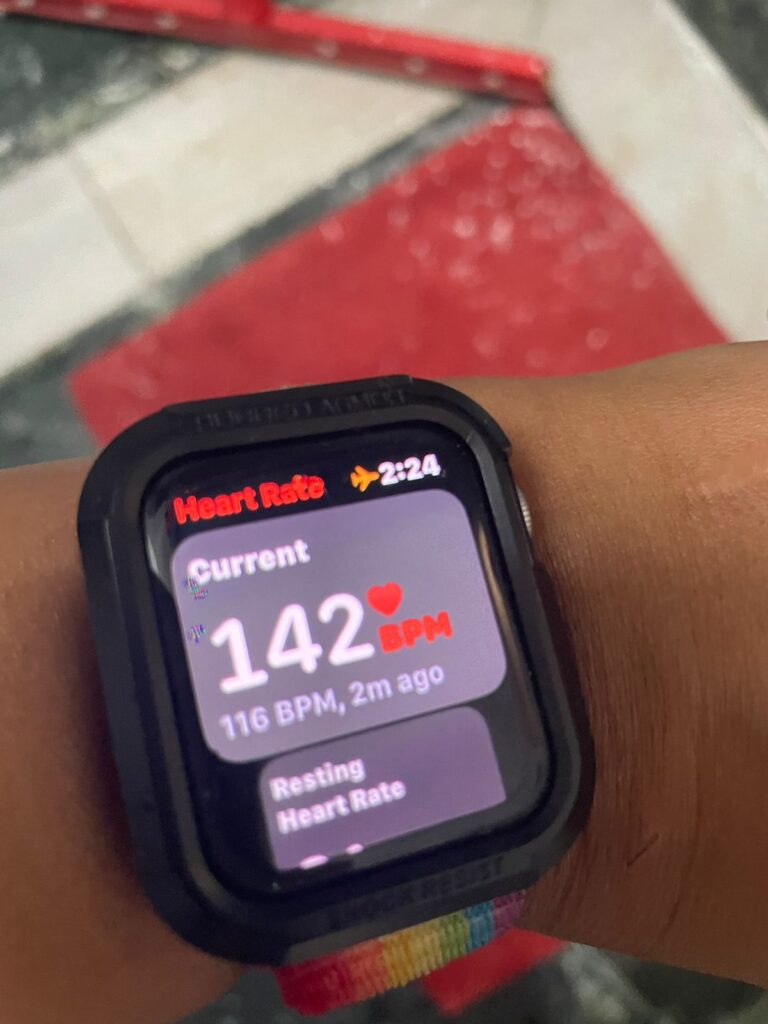
Long COVID dysautonomia causes POTS or postural orthostatic tachycardia syndrome, making it hard to stand up. Brushing my teeth can spike my heart rate to 150 beats, so I squat or sit down to do so. Sitting inclined is most comfortable, and lying down is best. I use my hiking poles as walking sticks. I bought a walker with a seat. Practicing pacing as a way of life is everything. PEM, or post-exertional malaise, and ME/CFS, or myalgic encephalomyelitis/chronic fatigue syndrome, validate what I feel.

Eight months later, in August 2022, I was exposed to COVID again. I tested negative, yet it felt like a re-infection. My long COVID symptoms of breathlessness, palpitations, and overwhelming fatigue returned with a vengeance. Thankfully, a long COVID research group educated me about “long COVID flare-ups.” The recovery is sinusoidal, like autoimmune inflammatory conditions. Symptoms are triggered by any insult, and hopefully, flares reduce with time until they fade and disappear altogether.
Reluctantly, I went on disability and haven’t been able to work since. I had to hire daily home help privately, costing me a hundred dollars a day. My insurance simply wouldn’t send me help. Social workers came and went, and I filled out so much paperwork. My loved ones took turns to help. Fourteen months into long COVID with dwindling savings, I finally moved in with family, which was the best decision ever.
My days begin with drinking 2 liters of salted water, checking vitals, doing breathwork, and putting on waist-length compression stockings. I can interact with 3-4 people a day, no more. Navigating my own medical care, insurance, and disability is a full-time job. Each time I try to exert myself even a bit more than I should, it sets me back. During flare-ups, I lie in a quiet, dark room to minimize sensory input until I feel better. Minor flare-ups improve in 2 to 3 days with rest and pacing. Major flare-ups are scary and take weeks to improve.
Recovery is a moving target while taking four steps forward and three backward. One doctor told me it would take me six months to recover, and another said I could possibly live like this for life. Once I reframed my expectations, I noticed improvements, even if it was at a snail’s pace.
I am lucky to have seen COVID specialists in New York City, South Africa, and India virtually. I managed to find long COVID survivors in my demographic who have recovered. I feel like a long COVID patient expert now.
When my Long-term disability was initially denied, it left me months without a paycheck. It was infuriating being told my symptoms were subjective when I had hard data to prove I had long COVID POTS and dysautonomia. It is such a reductive and strange roller coaster ride of emotions with fluctuating energy levels. Small joys, gratitude, and hopeful stories help me keep my head above water.
This is no death, but it is no life either. Going through the different stages of grief and being met with pity and sympathy isn’t fun. However, I am finally at a stage where acceptance has somewhat arrived. Thank goodness for my own wellness practices honed over the years and the incredible support from loved ones. Thank goodness for social media, through which I found much-needed support and validation. I am a privileged long hauler, uniquely positioned with access to the world’s best resources. This is a long road, and yet I have hope. I give myself a lot of credit for patiently meeting challenge after challenge while I try to meet my life graciously exactly where it is right now.